How
was your lockdown?
Reflections
of a therapist during the Covid-19 pandemic
Julia Samuel
Vice President, BACP; Founder Patron, Child Bereavement UK
Key words
lockdown, therapy, grief, debrief
I am
regularly asked 'how was your lockdown?'
It is a
good question. My brief answer is that I was busy. I did not make sourdough or
learn to play an instrument; I worked. Harder than I have
ever worked before.
In this
article I would like to explore what that meant at a deeper level, both
psychologically and practically; as a therapist, a
woman and my multiple other roles. What were my challenges and what helped me
keep my head above water? What have I learnt? I write this in the frame that 'the
personal is the most universal,' the wise words of Carl Rogers, in the hope
that you will identify aspects of yourself in my experience that may resonate
with you, or not. Whatever your response is, it might give you insight for your
own reflections – on your
role in this broad field of bereavement care and research.
*
In my
training, when asked that familiar question, 'why did I want to be a therapist?'
I moved quickly from that common, and not inaccurate, understanding 'I want to
help people, I like being needed' to recognising that
I gave what I most wanted to receive. Additionally, I became aware that being
in meaningful relationship was profoundly important to me. My curiosity was
fired by what was going on below the surface, rather than what people showed. I
came to see that being a therapist was by no means an altruistic endeavour but one that met my needs as well as having the
satisfying aim of supporting my clients. The roots of this
was certainly in my childhood and of course, being human; we are wired
to relate and connect. For over 30 years in my supervision and therapy I
regularly negotiate how those forces influence my practice. The reason I tell
you this is that the pandemic turned the volume up on all those responses. In
the crisis I had a greater drive to want to help, to meet the needs of others
and form close relationships.
This
initially showed itself by me offering to support a UK National Health Service
(NHS) team of medical staff working in an intensive care unit. Two consultants
liaised with me, and we decided on two lunchtime slots, of an hour, every week.
I would be one side of the Zoom call and the team would be in the staffroom
talking to me through a phone; taking it in turns to express the full gambit of
emotion that you can imagine someone would feel in that situation. For confidentiality
reasons I can only tell you my experience.
I gained a
lot from being useful. Being part of the NHS, even in this tiny way, gave me a
sense of belonging and purpose as we faced this crisis, which anchored me.
Fortunately, I was able to draw on decades of experience supporting medical
staff in the NHS, which has left large reserves of respect and warmth for all
health professionals. Those foundational responses stayed with me throughout
the tumult of the work and centred me – and I
think were felt by the team. We quickly developed the underlying key to a
therapeutic relationship – trust – and formed a working alliance.
It was
intense. My journal reminds me of some of my process: 'I always feel bad that
somehow I can't offer enough, but I was glad they talked ... so touched by the
care they give patients.' Another one: 'I was proud today, excellent session ...
they were emotionally honest, and it felt an important part of keeping the team
together ... we discussed some useful coping strategies.' Or, 'a painful
session, I was tense, worried that we all felt worse afterwards!' There were
nights I woke with anxiety from difficult images and stories. Wonderful moments
of black humour, raucous laughter, which sparked
warmth and connection and a defence yes, but also a
healthy protection in the face of the difficulties.
The
pandemic had thrown us all into an alien and frightening landscape of grief.
Grief is a messy, chaotic, unpredictable, subjective business. It often
switches our autonomic nervous system to code red. Part of my professional
practice is to find ways to keep myself centred when
those I'm working with are suffering. I use habits like exercise to balance me:
also theories as frameworks to turn to help me understand what is going on in
the therapy. My pivotal theory is the dual process model (Stroebe
& Schut, 1999). I like the dynamic oscillation
between restoration orientation and loss orientation, the movement between the
two. Allowing people to confront their pain and in restoration to avoid it.
Often people describe grief as hitting them in waves. This theory allows for
that, and allows for our natural survival mechanism, giving ourselves
opportunities to have a break from the pain, to be distracted, have a plan, and
most importantly have hope. It is hope that turns a life around. It discusses
gender norms; men tend to be restoration oriented, and women tend to be loss
oriented. I describe this theory to clients and told the ICU team about it;
they too found it helpful to have a theory that helped them understand and
accept themselves.
As I
reflected then, and with more clarity now, the team was my client. There was a
parallel process.
I felt as
powerless as them in the face of multiple difficult and traumatic deaths. (Of
course, they saved many lives as well.) We were all in the helping profession,
we wanted to make a difference and in our own way had to recognise
the limits of what we could offer; accept that simply being present is of value
– important. The curative power of listening,
witnessing, being alongside someone, offering heartfelt care. Although
working with many people was more of a psychological juggle, and it was
therapeutic rather than therapy,
I drew on
similar knowledge, skills and practice that I would with a one-to-one client.
The
emotional turmoil they lived was transferred through the screen to me, bodily.
I felt surges of fear which I acknowledged: 'gosh that's
frightening to even hear, it must have been...' and breathed into it, allow,
but not act on. It was my job to hold steady, to listen, be an empathic
presence who named the team's process; explore their individual difficulties,
listen as they expressed their feelings, gain insight and through the
collective sharing a normalisation of what they felt
– they weren't failing by being distressed. Helping them recognise not to conflate their feeling with fact; they may
feel they've failed if someone dies, but that does not make it so. Those
responses are common in my one-to-one therapy too. Often the first step with a
client is letting them know that however 'mad' or 'bad' they might feel, what
they are feeling is normal in grief. Rather than self-attack, which can be a
cruel default response in grief, encourage them to hold the messages from both
their head and heart side by side. Hold the discomfort of feeling guilty while
knowing they aren't actually guilty.
The team
had to go straight from the session into the intensive care unit, so it was
important to find a balance. As with all therapy it was a dance, of moving in and out – allowing and letting go. Using
myself as a reference point as to what was going on. Trusting my instincts on
how to respond, some worked, some didn't – I'd check what I missed and
reconnect. Sometimes offering practical ideas;
demonstrating breathing exercises, suggesting walks in nature. Using my voice
and presence to contain strong feelings. It was turbulent, with missteps from
me, but overall we did what we contracted to do: emotionally support the
individuals in the team, which built resilience in the whole team, to manage
themselves as they worked in the ICU.
Comparing
this to my individual clients; I would explore at
greater depth their internal process, perhaps use Gendlin's
(1982) felt sense to help them access their bodily wisdom. Working to align
their mind–body connection, to find both the narrative they are telling
themselves and what the emotional signals their body is transmitting to them
mean. Creating a safe place where they come to trust that, as difficult as it
is, pain is the agent of change. That paradoxically by allowing themselves to feel the pain of loss, voice it, express it,
is what over time allows them to heal. It is what they do to block and anesthetise their pain; alcohol, food, sex, or busyness to
name but a few, that over time leads to long-term negative consequences.
*
The demand
in my private practice was immense. My experience was that my clients'
pre-existing difficulties were intensified. If they had anxiety their fear
ramped up. If they were grieving, having their usual social support and
structures removed overnight meant many fell into despair. Some clients were
dying which meant the very precious time they had left was not spent with their
children or grandchildren, their last chance to be present at significant
events was cancelled. Everything medical was supremely challenging.
Those new clients who were bereaved through Covid
suffered traumatic grief; not being at the bedside, or the graveside, having no
rituals or connected support. Their sense of frozen surreal grief, agonising
as it was, is only now beginning to thaw. It will be a long road.
To sum it
up, I saw more suffering in the last 18 months than I have seen in my three
decades as a therapist. It was devastating. And their suffering was invisible,
locked away in people's minds and homes. The mental health
pandemic running beneath the health pandemic. I believe the greatest
psychological pain was inflicted by the isolation. When people we love die, we
need the love of others to help us survive. Their presence,
their hugs and, yes, their dishes of lasagne.
The path to recovery in grief needs to be paved with people and in the time of Covid it was a chilly emptiness. The fallout has not been
reckoned with and I have no doubt it will inform the content of our therapy
rooms for years ahead.
*
To finish on a personal note. I was unquestionably seduced by being needed; when I felt most overwhelmed by my own fear being busy and
useful was my defence to cope with it. I see again
(not exactly rocket science) that under duress I, and most of us, revert to
default modes of coping, and in the future really clocking that early might
enable me to make better informed choices.
I paid a
price for being that busy. I didn't see my family as much as I would have
liked. I wondered, did my clients get the best of me,
with my family getting the dregs? I felt guilty and it echoed earlier guilt as
a parent.
On the
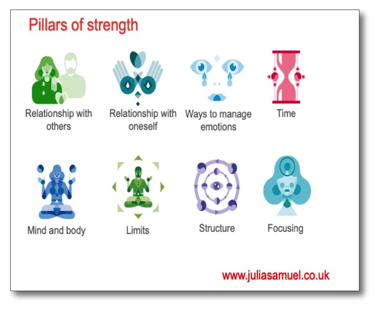
positive side I have good habits that enable me to stay sane and healthy. They
are based on my 8 Pillars of Strength (see below) where I take lots of exercise,
meditate, and am self-compassionate. My time boundaries held. I always stopped
work at a reasonable hour. I ate with my family, watched a great deal of only
happy television (much to my husband's irritation), and laughed and hugged
– a lot. That physical holding was emotionally vital for me.
What have I learnt? To state the obvious, crises are a complex, extreme
business. I found it demanding and rewarding in equal measure. I need to pay
attention to how seduced I can be by my work. It has magnified my respect for
the power of the human spirit. I am in awe of my clients, for both expressing
their pain and their strength.
How we
spend our days is how we spend our lives, time is precious. Use it mindfully.
I believe
more profoundly that love is what matters most.
Fundamentally
I am grateful for being in a profession that I truly love. To quote Freud, 'Love
and work, work and love is all there is.'
References
Gendling E (1982) Focusing. Bantam Books.
Stroebe MS & Schut HAW (1999) The dual process model of coping with bereavement: rationale and description. Death studies, 23(3) 197–224.
Further reading/resources
Action for Happiness www.actionforhappiness.org
Beattie G (2004) Visible thoughts: the new psychology of body language. Routledge.
Ben-Shahar T (2011) Happier: Learn the secrets to daily joy and lasting fulfillment. McGraw Hill.
British Psychological Society (2008) 2008 psychological debriefing www.who.int/mental_health/mhgap/evidence/resource/other_complaints_q5.pdf?ua=1
Damasio A (1999) The feeling of what happens: Body, emotion and the making of consciousness. Heinemann.
Department of Health (2005) When a patient dies. https://bereavementupdate.blogspot.com/2005/12/department-of-health-uk-when-patient.html
Duhigg C (2012) The power of habit. Random House.
Gibbs (1998) Reflection model. www.ed.ac.uk/reflection/reflectors-toolkit/reflecting-on-experience/gibbs-reflective-cycle
Kabat-Zinn J 2012 Mindfulness for Beginners: Reclaiming the Present Moment-and Your Life. Sounds True.
Kabat-Zinn J (2001) Full catastrophe living: How to cope with stress, pain and illness using mindfulness meditation. Doubleday.
Mehrabian A (1972) Nonverbal communication. Aldine-Atherton.
Mind (2017) Food and mood. www.mind.org.uk/information-support/tips-for-everyday-living/food-and-mood/about-food-and-mood
Pennebaker JW (2004) Writing to heal: A guided journal for recovering from trauma and emotional upheaval. New Harbinger Press.
Pennebaker JW (1997) Opening up: The healing power of expressing emotion. Guilford Press.
Samuel J (2017) Grief works: Stories of life, death and surviving. Penguin.
Schut HAW, Stroebe MS, Boelen PA & Zijerveld AM (2006) Continuing relationships with the deceased: Disentangling bonds and grief. Death Studies, 30, 757–766.
Schore A (2003) Regulation and the repair of the self. Norton Books.
Tedeschi RG & Calhoun LG (2012) Resilience: the science of mastering life's greatest challenges. Cambridge University Press.